Sub-fertility is a significant issue in Australia – around 16% of Australian couples have trouble conceiving, with both male and female-related issues affecting fertility rates. Fertility and preconception is an area of health that can feel entirely foreign when you begin trying to conceive, and the jumble of information available online can feel overwhelming. If you’re having difficulty conceiving, or even if you’ve only just begun your preconception journey, this article about fertility naturopath treatment will help you to understand some of the key factors that might be impacting on your fertility, as well as provide tips to help you boost fertility and help you to conceive naturally.
Female Fertility 101
Before getting into the factors which disrupt female fertility, it’s important to have a brief look at how fertility in women works on an anatomical and biochemical level, to help us understand what we’re dealing with (and how we can help to improve fertility outcomes).
In a normal menstrual cycle, a woman releases one egg (also known as an ovum or oocyte) from one of her ovaries into the fallopian tube – the process known as ovulation. It is here that the egg is able to be fertilised by sperm, before travelling through the fallopian tube and into the uterus, where the newly fertilised egg, now known as an embryo, implants into the endometrial lining of the uterus. The release of a healthy egg from the ovaries, as well as the development of a healthy endometrial lining for the embryo to implant in, requires a balance of hormones such as oestrogen, follicle-stimulating hormone, luteinising hormone, and progesterone, as well as adequate nutrients for the development of a healthy egg, embryo and endometrium. The factors that can interrupt this process are varied, and may affect just one portion of the process, or may impact the process as a whole.
Image by FreePik
Factors Affecting Fertility
So, what factors can impact on female fertility and conception? You may have an idea of some of the major factors, such as age, but there are many physical and lifestyle factors that can contribute, and you may find there are multiple issues you need to address when it comes to improving your fertility. Some of the major factors are:
- Age
- Genetics
- Nutrition
- BMI
- Stress and lifestyle
- Chemical/ toxin exposure
- Pre-existing medical conditions
Some of these, such as age and genetics, we unfortunately aren’t able to change, but there are many factors here that we can address.
Below is a more detailed look at some of these issues, and what we can do to help mitigate their effects.

How Can Nutrition Affect Female Fertility?
Nutrition is a huge area of focus when it comes to preconception and fertility. The old adage “you are what you eat” is particularly true for fertility. A poorly balanced diet, or one with specific nutrient deficiencies, leaves you without the key building blocks needed for successful conception and healthy foetal growth. Certain micronutrients, such as zinc, selenium, iron, iodine, B vitamins (especially folate and B12), and vitamin C (among others!) all play important roles in conception and embryonic development. Likewise, a balanced intake of macronutrients (protein, carbohydrates and fats) from healthy sources is essential. For example, eating a diet with too many high glycaemic index (GI) carbohydrate foods has been shown to increase insulin levels, which can contribute to an increase in the body’s production of androgens (“male” type hormones), disrupting normal hormone balances needed for successful conception.
Antioxidants are another important nutritional consideration, as a diet low in antioxidants is considered a risk factor for reduced fertility. Normal bodily processes as well as exposure to harmful chemicals in daily life contribute to the development of free radicals within the body, which lead to oxidative stress. Our bodies counteract the damaging effects of free radicals with antioxidant compounds that work to neutralise free radicals. Certain vitamins, such as vitamins C and E, as well as other nutritional compounds like glutathione, lycopene, resveratrol, and coenzyme Q10 (CoQ10), all act as important antioxidants within the body. It is vital that we are eating sufficient levels of these nutrients in order to keep the body in balance, especially when trying to conceive.
In addition, high caffeine intake has been shown to increase the risk of early spontaneous pregnancy loss, and studies have shown it to increase the time it takes to conceive. With that in mind, it’s best to skip the second (or third, or fourth) cup of coffee!

Improving Nutrition During Preconception
- Eat a balanced diet high in nutrient-dense foods and ensure you are eating adequate amounts of key fertility-boosting nutrients
- Plenty of fresh fruits and vegetables – aim for as much variety as possible, focusing on eating as many different colours of vegetables as you can each day (always be sure to wash your fruits and vegetables before consumption)
- Opt for high quality protein sources, such as wild caught fish, legumes, grass-fed organic meats and free-range eggs. Reduce your intake of highly processed meats such as sausages, and deli meats like ham and pastrami.
- Choose lower GI, wholegrain carbohydrates such as brown rice and wholegrain breads
- Boost your intake of key micronutrients for healthy conception
- Zinc: Found in beef, eggs, milk, seafood, sunflower seeds, pumpkin seeds, blueberries, broccoli and capsicum
- Selenium: Found in Brazil nuts, cashews, eggs, fish such as tuna, oysters and other seafood
- Iodine: Found in fish, kelp, mushrooms, dairy products and sunflower seeds
- Iron: Found in beef, chicken, eggs, spinach, tahini
- B vitamins: Found in green leafy vegetables, lentils and other legumes, avocado, mushrooms, sunflower seeds
- Vitamin C: Found in strawberries, oranges, broccoli, tomatoes, kiwi fruit, sweet potatoes
- Eat plenty of antioxidant-rich foods: fresh fruits and vegetables in plenty of different colours
- Reduce your caffeine intake, or avoid caffeine altogether

Can My BMI Affect My Fertility?
Being overweight or obese (BMI above 25), has been shown to reduce rates of conception and increase the risk of miscarriage. A high BMI is also associated with adverse pregnancy outcomes such as premature birth, hypertension, and gestational diabetes, further highlighting the importance of achieving and maintaining a healthy weight prior to conceiving.
Reducing the Effect of BMI on Fertility
The best way to approach this is to speak with your naturopath about a weight reduction plan appropriate to your needs. Remember that even a small reduction in body weight can help to improve ovulation and improve pregnancy outcomes.
Cigarette Smoking, Alcohol and Recreational Drugs
Cigarette smoking affects female fertility in a number of ways, including increasing the risk of spontaneous miscarriage and directly damaging eggs, reducing your ovarian reserve (i.e. the number and quality of eggs left in your ovaries). Although alcohol only indirectly affects fertility, foetal alcohol spectrum disorder is a major consideration in the recommendations for women abstaining from alcohol altogether when trying to conceive. Marijuana use can also affect fertility. Cannabinoids within marijuana have been shown to disrupt hormonal regulation and ovarian function, leading to ineffective implantation.
Reducing their Effects on Fertility
It is vital to eliminate cigarettes, alcohol and recreational drugs from your lifestyle while trying to conceive and during pregnancy and breastfeeding. With regards to cigarette smoke, it is also important to avoid second-hand smoke exposure, which can also be dangerous.

Stress
Both psychological and physical stress can play a role in reduced fertility in women. Stress activates the body’s hypothalamic-pituitary-adrenal axis (HPA axis), also known as the “flight or fight response”, leading to elevated levels of hormones such as cortisol. Over time these stress hormones negatively affect fertility by altering the body’s secretion of important fertility hormones like oestrogen and luteinising hormone, and altering ovulation, fertilisation, and implantation. This stress might include a physically or psychologically demanding job, or other types of stress such as relationship and family issues, insecure housing or employment, or financial stress.
Reducing the Effects of Stress on Fertility
The good news is that stress management techniques have been shown to help improve fertility outcomes. There are a range of options available to help reduce the effects of stress, including:
- Regular physical activity – aim for 30 minutes of moderate intensity exercise on most days of the week
- Yoga, tai chi, or Qi Gong
- Meditation – if you find the thought of self-guided meditation daunting, there are many group classes available nowadays, both in-person and online
- Counselling and talk therapy
Chemical and Toxin Exposure
It’s no secret that our modern world is full of harmful chemicals and toxins, to which we are exposed daily. Some of these toxins are particularly worrisome when it comes to preconception and it is worth looking into how we can avoid exposure. One of the primary reasons these chemicals are concerning during preconception is because of they way they can act as endocrine disruptors (sometimes also known as xenoestrogens), affecting hormone balance and disrupting the body’s ability to regulate its own hormones. They may also lead to increases in oxidative stress within the body, affecting healthy egg production. Chemicals that may impact fertility are:
- Pesticides, including garden sprays and herbicides, insect sprays and rodent baits
- Heavy metals, including mercury and lead, which can be present in contaminated water and food, as well as air pollution
- Certain plastics, such as phthalates and bisphenol-A (BPA)
- Chemicals in your cleaning products at home plus perfumes, make-up, shampoo & conditioner, hairsprays, toothpaste, skincare, soaps, body washes, hair dyes and nail-polish. Our blog on estrogen dominance goes into these chemicals in more detail, you can check it out here.
Reducing their Effect on Fertility
The best way to reduce their effect on fertility is to reduce your exposure:
- Avoid exposure to pesticides
- Choose organic gardening methods and avoid using Round-Up in your garden
- Wash fruits and vegetables thoroughly before eating and choose organic where possible
- Avoid exposure to heavy metals
- Use a water filter to reduce impurities and contaminants from tap water
- Reduce consumption of foods which may be contaminated with heavy metals, particularly fish such as shark, swordfish and bluefin tuna – opt for lower mercury varieties such as sardines, mackerel and salmon
- Avoid exposure to BPA and other harmful xenoestrogens
- Avoid plastic food containers and water bottles
- Do not microwave food in plastic containers – reheat foods on the stove top or in the oven, or if you do choose to use a microwave, use microwave-safe glass containers
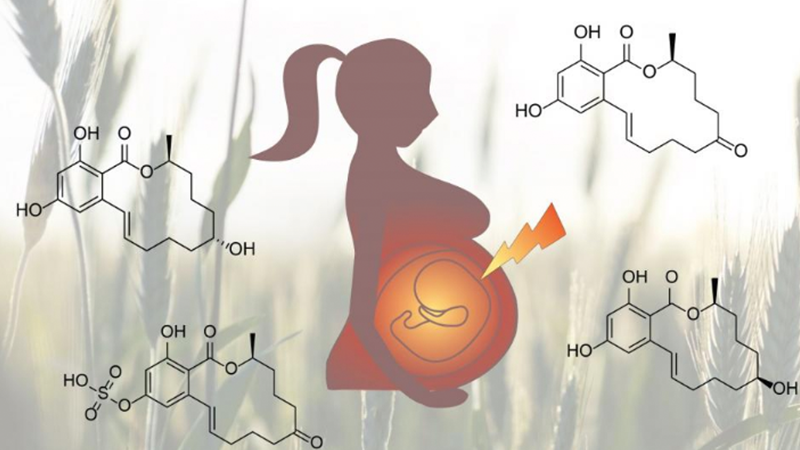
Image by University of Vienna
Pre-Existing Medical Conditions
There are a vast range of pre-existing medical conditions which can impact on fertility in women, whether as a result of the condition itself or through the medications and other treatments that may be used for the condition’s management. It’s beyond the scope of this post to list every condition that might affect female fertility, but a few of the major conditions, including female reproductive conditions, are listed below.
Some female reproductive conditions which may impact your fertility are:
- PCOS is a relatively common hormonal condition, affecting approximately 20% of women, which is associated with high levels of androgens (“male” hormones), which can disrupt ovulation, leading to “immature” eggs that don’t function as they should
- Endometriosis is a complicated hormonal condition that involves abnormal growth of the endometrium, which lines the uterus
- Uterine fibroids are a type of benign tumour within the uterus which cause a physical barrier to fertility. Depending on their exact location and manifestation, uterine fibroids may negatively affect implantation and increase the risk of miscarriage.
Other conditions to be aware of are:
- Infections, including sexually transmitted and genitourinal infections, may disrupt fertility in a number of ways. For example, sexually transmitted infections such as chlamydia can cause irreparable damage to the fallopian tubes, significantly impacting fertility. These infections can be asymptomatic, so it is important to speak to your GP about keeping up to date with STI screening.
- Thyroid disorders
- Diabetes
- Autoimmune conditions
Reducing their Effects on Fertility
If you have concerns about a diagnosed health condition or prescribed medications and how it may affect your plans to conceive, always speak with your naturopath or GP for advice. With regards to female hormonal conditions, your naturopath may also be able to prescribe herbs, such as shatavari, white peony, or chaste tree, to help mitigate the effects of the condition and improve hormonal regulation and promote ovulation.
Find out more about how we can support you through fertility and contraception – we are an award winning naturopath in Sydney’s Inner West, so please make contact or book an appointment.
References
Conforti, A., Mascia, M., Cioffi, G., De Angelis, C., Coppola, G., De Rosa, P., Pivonello, R., Alviggi, C., & De Placido, G. (2018). Air pollution and female fertility: A systematic review of literature. Reproductive Biology and Endocrinology, 16(117). https://doi.org/10.1186/s12958-018-0433-z
Family Planning NSW. (n.d.). Infertility. Retrieved February 22, 2021, from https://www.fpnsw.org.au/factsheets/individuals/fertility-and-infertility/infertility
Hechtman, L. (2012). Clinical naturopathic medicine. Elsevier Australia.
Lisiecki, M., Paszkowski, M., & Wozniak, S. (2017). Fertility impairment associated with uterine fibroids: A review of the literature. Menopause Review, 16(4), 137–140. https://doi.org/DOI: https://doi.org/10.5114/pm.2017.72759
Palomba, S., Daolio, J., Romeo, S., Battaglia, F. A., Marci, R., & La Sala, G. B. (2018). Lifestyle and fertility: The influence of stress and quality of life on female fertility. Reproductive Biology and Endocrinology, 16(113). https://doi.org/10.1186/s12958-018-0434-y
Rattan, S., Zhou, C., Chiang, C., Mahalingam, S., Brehm, E., & Flaws, J. A. (2017). Exposure to endocrine disruptors during adulthood: Consequences for female fertility. Journal of Endocrinology, 233(3), R109–R129. https://doi.org/DOI: 10.1530/JOE-17-0023
Silvestris, E., Lovero, D., & Palmirotta, R. (2019). Nutrition and female fertility: An interdependent correlation. Frontiers in Endocrinology, 10(346). https://doi.org/10.3389/fendo.2019.00346











