You’ve heard the term but what does it mean?
Endometriosis is a complex, painful female reproductive condition that affects around 1 in 9 women worldwide. So, there is a high chance someone in your friendship circle suffers from it.
We understand that in a normal cycle our tissues respond to hormones and prepares the uterus for pregnancy. When pregnancy does not occur, the lining breaks down, sheds, and creates a menstrual bleed.
For someone with endometriosis, tissue will implant in areas outside of the uterus, usually on pelvic organs such as the ovaries, bladder and bowels, or on other pelvic tissues. These cells grow and form deposits or lesions of tissue. Although not quite the same as endometrial tissue, this tissue reacts similarly to hormonal changes, growing and proliferating and then eventually breaking down, bleeding into the pelvic cavity. The blood and broken-down tissue are trapped inside the pelvic cavity, causing inflammation, irritation, and significant pain.
The condition can significantly impact a person’s life, and what’s worse, diagnosis is often delayed – it takes an average of 6.5 years for a person to receive this diagnosis. Identification of endometriosis is generally via laparoscopy, a type of keyhole surgery that is also used to remove endometriotic tissue.

Signs and Symptoms of Endometriosis
One of the most common key symptoms of endometriosis is period pain, which is often severe and can significantly impact quality of life. In addition to period pain, endometriosis sufferers may also experience:
- Heavy menstrual bleeding
- Bleeding between periods
- Rectal bleeding, or blood in the urine
- Fertility issues
- Pain during or after sex
- Lower back pain
- Painful bowel movements
- Because of the significant impact endometriosis can have on quality of life, it is also associated with increased depression and anxiety
What Causes Endometriosis?
Endometriosis is a complex condition and is not yet fully understood.
One of the most common theories for how these endometrial-like cells find their way into in the pelvic cavity is that of “retrograde menstruation”. This is where small fragments of menstrual blood flow up the fallopian tubes and into the pelvic cavity. It is thought that several different mechanisms, such as hormones, inflammation, genetics, and immune dysregulation, then play a role in these tissues attaching to areas of the pelvic cavity and becoming responsive to the hormonal changes of the menstrual cycle.
Factors that are associated with endometriosis include:
Hormonal Imbalances
Endometriosis is often called an “oestrogen-dependent condition”. Endometriotic lesions respond differently to hormones and can lead to increased production of oestrogen compared to progesterone, also known as “oestrogen dominance”. These higher than normal levels of oestrogen further increase the growth of the lesions in endometriosis and also increase inflammation and pain, and impact fertility.
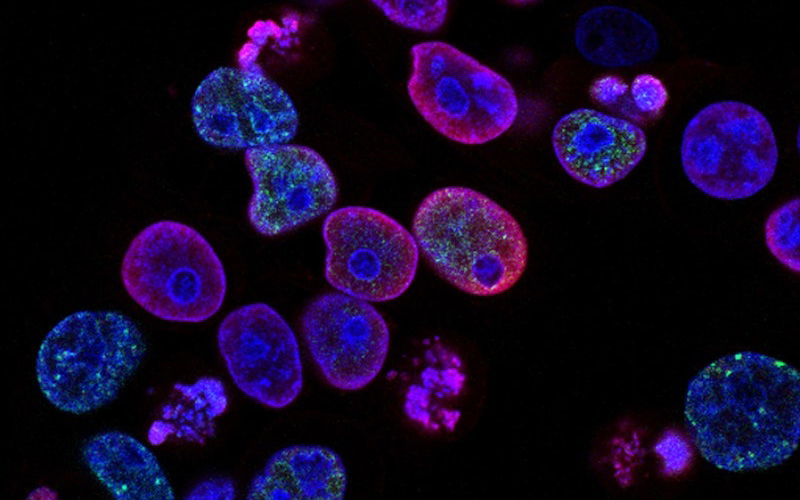
Immune Activation
Increased levels of a number of different T cells (a type of immune cell) have been shown in endometriosis, suggesting immune dysregulation plays a role in endometriosis. These immune cell changes are associated with increased inflammation and higher than normal levels of inflammatory cytokines. Pre-existing immune dysregulation and autoimmune conditions may be a risk factor for endometriosis.
Leaky Gut and Dysbiosis
Changes to the microbes in our intestines, called dysbiosis, can lead to inflammation and “leaky gut”, where the lining of the intestine becomes less tightly sealed, allowing for harmful inflammatory proteins to enter circulation. Dysbiosis can also affect hormonal balance and immune system function. Studies have shown those with endometriosis to have significantly altered gut microbiome, and a 2020 study showed women with endometriosis have higher than normal intestinal permeability. These studies suggest the microbiome may play an important role in the development of endometriosis and may also be involved in the increased inflammation associated with the condition.
Oxidative Stress
Endometriosis is associated with increased oxidative stress, which may in part be due to intestinal dysbiosis and leaky gut, which increase inflammation and oxidative stress.
Genetics
Family history of endometriosis increases the risk of developing the condition, suggesting that genetics play a role.
Naturopathic Treatments for Endometriosis
The good news is that there are a range of different naturopathic treatments that can be used to help with endometriosis. The specific remedies your practitioner uses will depend on your overall health, your specific symptoms, as well as other conditions you may also have. As always, it is important to speak with your naturopath before using these treatments, to make sure they are right for you.
Dietary Changes
Diet can play a big part in helping to reduce some of the symptoms of endometriosis, by helping to reduce some of the inflammation and oxidative stress.
Antioxidants
With increased oxidative stress associated with endometriosis, including antioxidant-rich foods in your diet is an important step in helping to reduce endometriosis symptoms. Include plenty of fresh fruits and vegetables in your diet and include foods of varying colours to help make sure you are eating a variety of different antioxidant compounds. Specific antioxidants, such as resveratrol (found in grapes and blueberries) and epigallocatechin (found in green tea), as well as vitamins such as vitamin C and vitamin E, can be particularly beneficial.

Anti-Inflammatory Foods
Similarly, focusing on increasing anti-inflammatory foods (and reducing foods that trigger inflammation), is important. Choose fresh fruits and vegetables, nuts and seeds, and quality sources of protein such as legumes, lean meats, and fish. Avoid foods and drinks such as alcohol, caffeine, excess sugar, and saturated or trans-fatty acids, which can all increase inflammation.
Fibre
Fibre is important for helping to maintain hormonal balance, as it binds excess oestrogen in the body so that it can be excreted. Fibre also provides fuel for healthy microbes in the gut, so can help to improve the gut microbiome. Increase fibre intake slowly, to avoid exacerbating symptoms of bloating, which can contribute to abdominal pain. Try adding psyllium husk or ground linseeds to your smoothies or sprinkled on top of Greek yoghurt. Eating fruits and vegetables with their skins on can also help boost your fibre intake (but be sure to thoroughly wash them first!).
Omega 3 Fatty Acids
Omega 3 fatty acids are important for reducing inflammation and inflammatory pain. Including omega 3 fatty acids in your diet can help to reduce the inflammation and pain associated with endometriosis. In fact, a recent double-blind pilot study found supplementation of omega 3 fatty acids for 8 weeks helped to reduce pain and improve quality of life in women with endometriosis. Choose fish such as salmon or sardines, as well as walnuts, chia seeds and flax seeds.
Vitamin D
Vitamin D is an important nutrient for immune regulation, and studies have shown that women with endometriosis have lower than normal levels of vitamin D. Sunlight exposure is the best way to boost your vitamin D levels – even 15 minutes per day can be beneficial. Vitamin D can also be found in free range eggs and oily fish such as salmon. If your vitamin D levels are very low, you may benefit from supplementation.

Probiotics
As discussed above, the gut microbiome may play a role in endometriosis, so helping to improve the microbial balance in the gut is important. Probiotics can also help to reduce bloating, which may exacerbate abdominal pain.
Iron
If you experience heavy bleeding because of endometriosis, you may be at risk of iron deficiency. Speak to your naturopath about whether an iron supplement may be right for you.
Herbal Medicines
In addition to dietary changes, there are also specific herbal medicines that can help with endometriosis.
Lady’s Mantle
Lady’s mantle is a herb with astringent qualities, that can be very useful in helping to reduce heavy menstrual bleeding.
Wild Yam
Wild yam is a herb used for its pain-relieving properties and is helpful for cramping pains such as menstrual pain.
Rehmannia
Rehmannia is a Chinese herb that has several important properties that make it useful in endometriosis. The herb is anti-inflammatory and also helps with immune regulation. Rehmannia is also useful for supporting liver function, so that the liver can detoxify and remove waste products, such as excess oestrogen.
Vitex
Vitex is a hormone-modulating herb. It can be used in endometriosis to help balance hormones and reduce elevated oestrogen levels.
If you are looking for naturopathic support for endometriosis, book your appointment with Tanya now to discuss treatment strategies and start feeling better.
References
Abokrhais, I. M., Denison, F. C., Whitaker, L. H. R., Saunders, P. T. K., Doust, A., WIlliams, L. J., & Horne, A. W. (2019). A two-arm parallel double-blind randomised controlled pilot trial of the efficacy of omega-3 polyunsaturated fatty acids for the treatment of women with endometriosis-associated pain (PurFECT1). PLOS One, 15(1).
Anderson, G. (2019). Endometriosis pathoetiology and pathophysiology: Roles of vitamin A, estrogen, immunity, adipocytes, gut microbiome and melatonergic pathway on mitochondria regulation. Biomolecular Concepts, 10(1).
Chapron, C., Marcellin, L., Borghese, B., & Santulli, P. (2019). Rethinking mechanisms, diagnosis and management of endometriosis. Nature Reviews Endocrinology, 15, 666–682.
Endometriosis Australia. (2020). Endo facts. https://www.endometriosisaustralia.org/research
Hechtman, L. (2012). Clinical naturopathic medicine. Elsevier Australia.
Marquardt, R. M., Hoon Kim, T., Shin, J.-H., & Jeong, J.-W. (2019). Progesterone and estrogen signaling in the endometrium: What goes wrong in endometriosis? International Journal of Molecular Sciences, 20(15).
Svensson, A., Brunkwall, L., Roth, B., Orho-Melander, M., & Ohlsson, B. (2021). Associations between endometriosis and gut microbiota. Reproductive Sciences.
Vigano, D., Zara, F., Pinto, S., Loddo, E., Casula, L., Soru, M. B., D’Ancona, G., D’Alterio, M. N., Giuliani, C., Angioni, S., & Usai, P. (2020). How is small bowel permeability in endometriosis patients? A case control pilot study. Gynecological Endocrinology, 36(11).










