Introduction
You may have heard the term “insulin resistance” before, particularly when it comes to reducing risk factors for common health conditions. But what exactly is insulin resistance, and how does it really affect your health? In this week’s blog post, we will be examining the role of insulin in the body and the effects of insulin resistance on health and wellness. We will also explore ways to help reduce your risk of developing insulin resistance and improve insulin function for better wellbeing.
What is Insulin and What Does it Do?
Insulin is our main hormone for controlling blood sugar levels in the body. It is a crucial hormone for normal body functioning, as it is the main way for the cells in our bodies to receive glucose (sugar) for energy. Insulin is also important for telling the liver to store glucose for later use. Insulin is particularly important for muscles, liver and fat cells – it is these cells which are most affected by insulin resistance.
Most cells in our bodies require glucose in order to function – it is the main energy source our cells use to perform their normal functions (and keep us alive!). However, too much glucose inside a cell can cause issues, so the amount of sugar entering the cell needs to be carefully controlled. Enter, insulin. Insulin molecules are released by the pancreas when extra sugar is detected in the blood stream (e.g., after eating). The insulin then circulates throughout the body via the blood. These insulin molecules bind onto the outside surface of cells and act like a “key” to unlock a passageway for glucose to enter the cell. Once glucose has entered, the insulin detaches from the cell wall to prevent too much sugar moving into the cell. The pancreas will keep producing/ releasing insulin until glucose levels in the blood return to normal. In this way, our body can carefully control blood sugar levels to ensure we have the energy needed for optimal function, without sugar levels becoming dangerously high.
In addition, insulin is a fat-storage hormone, meaning that high levels of insulin and insulin resistance may result in weight gain and elevated triglycerides.
Insulin Resistance
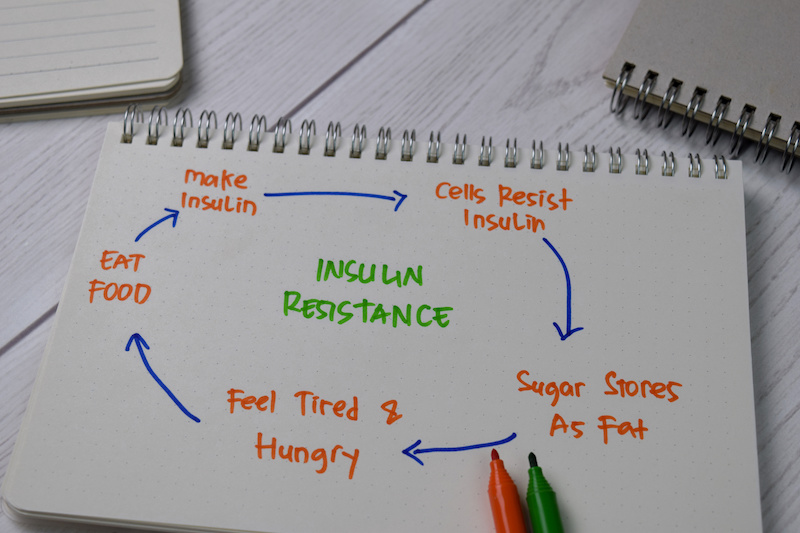
Insulin resistance is a condition where the body becomes resistant to the effects of the glucose-regulating hormone insulin, resulting in prolonged periods of high blood sugar. It is often asymptomatic, but left unchecked, it can progress to serious health issues including diabetes and metabolic syndrome. Insulin resistance can also occur due to other underlying health conditions, such as PCOS or Cushing’s disease. So, what causes insulin resistance and how can we reduce our risk of developing it?
How does insulin resistance develop? Essentially, when blood sugar levels remain high (as can occur with continued excess sugar consumption), the pancreas compensates by continuing to produce more and more insulin in an attempt to get blood sugar levels back down to a safe level. Eventually, the prolonged presence of insulin in the blood stream leads to cells becoming less responsive to insulin. This means more and more insulin needs to be produced in order to prompt cells to properly uptake the glucose present in the blood. Eventually, our cells are no longer able to use the insulin or to uptake glucose as effectively as before, and as a result, glucose levels in the blood remain high. This is known as insulin resistance.
Symptoms of insulin resistance
Insulin resistance can be completely asymptomatic, so many people are unaware there is an issue. However, some symptoms may include:
- Acanthosis nigricans – darkening of the skin under the armpits, in the groin, or even at the back of the neck
- Irregular menstruation – insulin resistance can disrupt normal hormone balance
- Excess thirst and frequent urination – due to your kidneys attempting to filter out the excess glucose in your blood
- Fatigue
- Skin tags
- Recurrent or chronic infections
- Gaining weight easily or an inability to lose weight
- Anxiety and feeling irritated commonly referred to as “hangry”
Risk factors for developing Insulin Resistance
There are a number of risk factors that can contribute to or increase your risk of developing insulin resistance. Addressing these risk factors where possible can reduce your overall risk of developing insulin resistance and other cardiovascular conditions.
Sedentary Lifestyle/ Low Physical Activity
Our skeletal muscles are one of the biggest users and storers of glucose. Physical activity is required for our muscles to use up their glucose stores, ready to absorb the glucose from the foods we eat. Inadequate physical activity means our muscles aren’t using up any glucose, leaving too much glucose circulating in the blood.
Being Overweight or Obese
Being overweight or obese, particularly if you carry your excess weight in your abdomen, can increase your risk of insulin resistance, as fatty tissue (especially abdominal fatty tissue) secretes hormones that promote insulin resistance.
High Glycemic Load & highly processed carbohydrate diet
Eating a diet that is rich in high glycemic loaded foods which includes processed carbohydrates cause powerful spikes in blood sugar levels and this leads to an increased risk of insulin resistance.

Smoking
Cigarette smoking and nicotine use directly increase insulin requirements and insulin resistance in a dose-dependent manner, meaning the more heavily you smoke, the greater the impact on insulin.
Sleep Issues
Turns out our circadian rhythm – the internal clock that keeps us awake in the day and make us sleepy at night – also influences blood sugar levels. When our circadian rhythm is disrupted (such as through ongoing insomnia/ sleep issues or shift work), it alters not only our sleep-wake behaviours but also our food intake, the sensitivity of muscles and fat tissue to insulin, and even the production of insulin in the pancreas itself.
Stress
Stress turns on our fight-or-flight response and puts us into a state known as parasympathetic dominance, increasing cortisol so the body is ready to respond to perceived threats. Unfortunately, when in parasympathetic dominance, the body down-regulates certain biological activities such as digestion, and also reduces the body’s sensitivity to insulin. From a biological point of view, this makes sense, as it means the glucose in our blood stream is readily available for rapid uptake to the muscles if we find ourselves needing to physically run from a threat. However, the chronic types of stress we encounter in the modern world don’t require us to physically run away from danger, so our glucose levels remain high, impairing the function of insulin.
Genetics
A number of hereditable genetic mutations have been identified that increase the risk of both insulin resistance and diabetes.
Health Effects of Insulin Resistance
The health effects of insulin resistance are due to the presence of excessive amounts of glucose in the bloodstream, which damages cells and disrupts normal body functioning, including hormonal balance and cell signalling.
Insulin resistance and high blood sugar can lead to:
- Inflammation – animal studies have shown that insulin resistance leads to an increased production of inflammatory molecules and activates inflammatory pathways in the body. Conversely, chronic inflammation can itself lead to reduce insulin sensitivity in cells, further exacerbating insulin resistance.
- Increased blood pressure – insulin can trigger sodium retention and also affects blood vessels, contributing to higher blood pressure.
- Abnormal cholesterol levels – insulin resistance prompts the body to produce more cholesterol and have lower levels of the good HDL cholesterol
- An inability to lose weight
- Brain fog, mood changes and cognitive issues – studies have demonstrated that insulin resistance can lead to reduced cognitive function, at least partly due to its effect on blood vessels, as well as the effects of high blood sugar on mood.
Insulin Resistance and Other Health Conditions
Insulin resistance doesn’t exist just on its own. Whilst diabetes is the most commonly thought of condition associated with insulin resistance, there are several other health conditions that can contribute to, or be exacerbated by insulin resistance, including polycystic ovarian syndrome (PCOS), non-alcoholic fatty liver disease, and even hypothyroidism. Insulin resistance also forms part of the symptom picture of metabolic syndrome, also known as syndrome X. Insulin resistance also leaves us more prone to other health conditions, including cardiovascular disease. Recent research also suggests a potential link between insulin resistance and an increased risk of developing Alzheimer’s disease in later life.
Diabetes
One of the most common health conditions associated with insulin resistance is diabetes. There are two types of diabetes – type 1, which is an autoimmune condition that most often begins in childhood or early adulthood, and type 2, which is classed as a “lifestyle condition”. This second type of diabetes more commonly begins well into adulthood, as a result of ongoing sugar consumption in excess of what our bodies are able to effectively process with insulin. Type 2 diabetes is essentially the disease state that results from ongoing insulin resistance – the pancreas becomes too fatigued to be able to produce sufficient insulin anymore and blood glucose levels cannot be controlled. For more information on type 2 diabetes, check out my blog post here.
Non-alcoholic fatty liver disease (NAFLD)
This is a condition that involves the accumulation of fat in the liver in individuals who do not consume an excessive amount of alcohol with scientific studies establishing that insulin resistance plays a major role in this disease.
PCOS
Insulin resistance is a common factor in PCOS, however there is contention regarding whether PCOS leads to insulin resistance or vice versa. PCOS is a complex and multifactorial condition, however there is a clear role of insulin resistance in the disease for many women. Insulin resistance contributes to PCOS because of the hormonal effects of insulin on the body. Insulin stimulates the production of androgens (“male” type hormones) and also increases inflammation in fatty tissues, which leads to fatty tissues converting oestrogen into androgen, leading to excess androgens and the development of PCOS symptoms.
Thyroid Conditions
The thyroid is an important organ for metabolism and energy use, so it’s no surprise that thyroid conditions and insulin resistance can be linked. In fact, thyroid hormones play a role in regulating insulin levels. Hypothyroidism in particular is associated with higher insulin levels and insulin resistance, and studies have shown that even subclinical hypothyroidism (that is, low thyroid function that might not necessarily be low enough for a standard diagnosis) can lead to insulin resistance.
Menopause
Menopause, although not so much a health condition as it is a normal life phase, is also associated with changes to insulin sensitivity due to the hormonal and metabolic changes that occur during this time. Oestrogen is involved in insulin sensitivity and balancing glucose levels, and naturally declines during menopause, leading to poorer insulin function and an increased risk of insulin resistance. This is also a time when many women will gain weight around their abdomen, which increases insulin resistance as discussed above.
Testing for Insulin Resistance
There are a number of different types of tests that can be used to assess insulin function. It is common that you have had fasting glucose tested previously and it is only when this is elevated that further testing is performed. As a naturopath, I need to understand what your insulin is doing behind the scenes to keep blood glucose levels normal. Based on your symptoms, I will often request further testing to assess this. Checking thyroid levels, hormone levels, liver function, cholesterol and triglycerides can also provide valuable information.
Naturopaths typically use more in-depth testing to assess for insulin resistance, as well as to obtain a more complete symptom picture to understand the underlying root cause of your condition.
Managing Insulin Resistance
Fortunately, there are plenty of dietary and lifestyle strategies that can help to combat insulin resistance and reduce the risk of developing conditions such as diabetes, weight gain, or PCOS.
With so many possible components to the development of insulin resistance, one size does not fit all with this condition and a review of your unique health situation including family history is highly recommended. Some basic tips that are helpful include:

Dietary Strategies
Eat regularly and avoid skipping meals
Eating regular, healthy meals will prevent excessive rises and falls in blood sugar (and will also help to prevent sugar cravings!)
Include protein in every meal
Protein helps to keep you full and also helps to slow down the uptake of sugar from meals. Slower sugar absorption means avoiding rapid spikes in blood sugar, which can trigger excessive insulin output from the pancreas
Eat plenty of fruits, vegetables and spices
Fruits, vegetables and spices are rich in antioxidants, which can help to reduce inflammation associated with insulin resistance. Fruits and vegetables are also an excellent source of fibre which can help to slow down sugar absorption
Other Management Strategies
Exercise daily
As we discussed above, our muscles are one of the main users of glucose in the body, so we need to be using our muscles to make sure we are making actually utilising the sugars in the foods we eat. Exercise also make cells more sensitive to insulin. 30 minutes of moderate intensity exercise (strenuous enough that you break a sweat) is a great place to start.
Focus on quality sleep
Insomnia is associated with insulin resistance so keep a regular sleep schedule and avoid disruption to your normal circadian rhythm.
Reduce your exposure to artificial lights and bright screens at night
Promote optimal circadian function by ensuring adequate sunlight exposure in the mornings (before 10am)
For additional tips on sleep click here
Quit smoking
Smoking directly increases the risk for insulin resistance
In addition to dietary and lifestyle changes, as a naturopath I prescribe herbs and nutritional supplements to help support your insulin function, depending on the underlying causes of your insulin resistance. As always, it is important to discuss your current medications and any diagnosed health conditions before taking herbs or supplements.
References
Baptiste, C. G., Battista, M.-C., Trottier, A., & Baillargeon, J.-P. (2010). Insulin and hyperandrogenism in women with polycystic ovary syndrome. The Journal of Steroid Biochemistry and Molecular Biology, 122(1–3), 42–52.
Brown, A. E., & Walker, M. (2016). Genetics of insulin resistance and the metabolic syndrome. Current Cardiology Reports, 18.
Bugianesi, E., Moscatiello, S., Ciaravella, M. F., & Marchesini, G. (2010). Insulin resistance in nonalcoholic fatty liver disease. Current pharmaceutical design, 16(17), 1941–1951. https://doi.org/10.2174/138161210791208875
Czech, M. P., Tencerova, M., Pedersen, D. J., & Aouadi, M. (2013). Insulin signalling mechanisms for triacylglycerol storage. Diabetologia, 56(5), 949–964. https://doi.org/10.1007/s00125-013-2869-1
Chiolero, A., Faeh, D., Paccaud, F., & Cornuz, J. (2008). Consequences of smoking for body weight, body fat distribution, and insulin resistance. The American Journal of Clinical Nutrition, 87(4), 801–809.
Ferreira, L. S. S., Fernandes, C. S., Vieira, M. N. N., & De Felice, F. G. (2018). Insulin resistance in Alzheimer’s disease. Frontiers in Neuroscience.
Geroldi, C., Frisoni, G. B., & Paolisso, G. (2005). Insulin resistance in cognitive impairment: The InCHIANTI study. Archives of Neurology, 62(7), 1067–1072.
Petersen, M. C., & Shulman, G. I. (2018). Mechanisms of insulin action and insulin resistance. Physiology Reviews, 98, 2133–2223.
Shimobayashi, M., Albert, V., Wolnerhanssen, B., Frei, I. C., Weissenberger, D., Meyer-Gerspach, A. C., Clement, N., Moes, S., Colombi, M., Meier, J. A., Swierczynska, M. M., Jeno, P., Beglinger, C., Peterli, R., & Hall, M. N. (2018). Insulin resistance causes inflammation in adipose tissue. The Journal of Clinical Investigation, 128(4), 1538–1550.
Shoelsen, S. E., Lee, J., & Goldfine, A. B. (2006). Inflammation and insulin resistance. The Journal of Clinical Investigation, 116(7), 1793–1801.
Stenvers, D. J., Scheer, F. A. J. L., Schrauwen, P., la Fleur, S. E., & Kalsbeek, A. (2019). Circadian clocks and insulin resistance. Nature Reviews Endocrinology, 15, 75–89.
Vyakaranam, S., Vanaparthy, S., Nori, S., Palarapu, S., & Bhongir, A. V. (2014). Study of insulin resistance in subclinical hypothyroidism. International Journal of Health Science Research, 4(9), 147–153.