Firstly, let me start by saying that this blog has been written to provide support to men with mild to moderate symptoms caused by having an enlarged prostate and for men who wish to initiate prevention strategies in their thirties or forties due to complications seen in older family members. As symptoms with this condition often worsen gradually over time, making important changes at early onset can be very helpful.
In the more severe and advanced cases of Benign Prostatic Hyperplasia (BNP), your GP will refer you to a specialist as chronic lower urinary tract symptoms including the inability to completely empty the bladder, increases the risk of kidney damage.
When supporting men with uncomfortable urinary tract symptoms that impact their quality of life, using a screening tool to assess the severity of their symptoms is a sensible place to start. I like to refer to The International Prostate Symptom Score (IPSS) with my clients which is an eight-question weighted survey that helps determine if symptoms are mild, moderate or severe.
Whilst I regularly work collaboratively alongside General Practitioners, it is not uncommon for me to refer my clients to a GP as part of my duty of care and to exclude other medical causes.
What is Benign Prostatic Hyperplasia (BPH)?
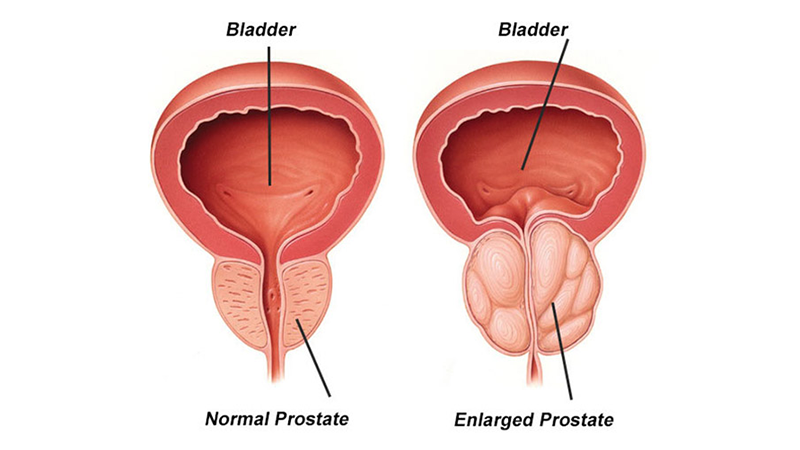
The prostate gland is a small muscular organ the size of a walnut that sits underneath your bladder and encircles the upper part of your urethra which is the tube that carries urine from your bladder to your penis. As this tube passes through the middle of your prostate, urine flow can be blocked when your prostate becomes larger and this tube (urethra) then becomes compressed.
Most medical experts agree that if a man lives long enough, they are almost 100% guaranteed of having their prostate enlarge. This only becomes an issue when this enlargement starts to cause lower urinary tract symptoms. Some men are fortunate enough not to experience these symptoms however the majority will experience some symptoms in their lifetime.
Benign prostatic hyperplasia (BPH) refers to the nonmalignant growth of the prostate gland as men age with studies around the world indicating that it takes place in 10% of men in their 30s, 20% of men in their 40s, 50-60% of men in their 60s, and 80% to 90% of men in their 70s and 80s.
It must be highlighted, however, that not all men with an enlarged prostate will go on to develop frustrating lower urinary tract symptoms. The reverse is also true meaning that some men may experience significant lower urinary tract symptoms without prostate enlargement (benign prostatic hyperplasia). In these cases, other conditions such as prostatitis, bladder or kidney stones, urinary tract infections and other disorders need to be excluded.
Image by Urology Specialist
What are common symptoms of Benign Prostatic Hyperplasia?
The severity of your symptoms is not always directly related to the size of your prostate. It can depend on where the growth has occurred meaning that sometimes only a slight enlargement may cause substantial symptoms, whilst much larger prostates may only cause minor issues.
Some of the more common symptoms are:
- Frequent urination
- A sudden and urgent need to urinate
- Nocturia: increased times you get up out of bed at night to urinate
- Incontinence
- Difficulty starting and straining to urinate
- A reduced force of urine stream
- A urine stream that is interrupted with stops and starts
- Dribbling once urination is finished
- A feeling of incomplete emptying of your bladder
- Urinary tract infections and painful urination
- Inability to urinate or only urinating small volumes
- Blood in your urine

What causes Benign Prostatic Hyperplasia?
Whilst this can be complex, an imbalance of hormones is thought to be involved in the growth of the prostate. Specifically, an increase in levels of a potent hormone called dihydrotestosterone (DHT) which is created from testosterone by an enzyme called 5-alpha reductase enzyme. Unfortunately, DHT is thought to be up to ten times more powerful in its stimulatory effect on prostate growth than testosterone.
Estradiol, a type of estrogen is thought to be another player in prostate growth. Estrogen is converted from testosterone by an enzyme in fat cells called aromatase. This is why obesity, metabolic syndrome, increased levels of blood insulin, diabetes, low levels of physical activity and diet are always a focus when developing naturopathic treatment aims. This estrogen dominance in the face of dropping testosterone levels is thought to be implicated.
Environmental exposure to chemicals called xeno-estrogens are thought to also act as hormone disruptors in this condition. This means they mimic estrogen and estrogen makes things grow.
Inflammation and high cholesterol are also thought to be a key component in prostate enlargement and the progression of benign prostatic hyperplasia (BPH).

What Naturopathic Treatment Aims Can You Expect for Prostate Health?
Natural medicine and naturopathic strategies have a great deal to offer in the prevention and treatment of Benign Prostatic Hyperplasia (BPH). Here are several worth highlighting:
- Regulating hormones: using diet, lifestyle guidance, supplements and herbal medicines to regulate hormones specifically the conversion of testosterone to potent DHT and estrogen is crucial. A combination of herbs may include Serenoa repens (Saw Palmetto), Urtica Dioica root (Stinging nettle) & Crataeva Nurvula (Crataeva). Guidance in regard to estrogen mimicking chemicals to avoid is another.
- Supporting the achievement of healthy weight and increased physical activity.
- Reducing inflammation in the body through the protective role of antioxidants can be achieved with an emphasis on particular foods and herbal medicines.
Naturopath’s have a number of dietary recommendations including:
- Zinc rich foods due to zincs role in reducing the conversion of testosterone to DHT;
- Fatty fish, nuts & seeds due to their anti-inflammatory effect;
- Reduced beer consumption. Beer increases a hormone called prolactin which is associated with prostate growth;
- Adding phyto-estrogen foods which block stronger estrogens and help to balance hormones. Flaxseed, freshly ground is a personal favourite.

To find out more about how we can support you through Benign Prostatic Hyperplasia, please book an appointment.
References
Ajayi, A., & Abraham, K. (2018). Understanding the role of estrogen in the development of benign prostatic hyperplasia. African Journal of Urology, 24(2), 93–97. doi:10.1016/j.afju.2018.01.005
Boyle, P., Robertson, C., Lowe, F., & Roehrborn, C. (2004). Updated meta-analysis of clinical trials of Serenoa repens extract in the treatment of symptomatic benign prostatic hyperplasia. BJU international, 93(6), 751–756. https://doi.org/10.1111/j.1464-410X.2003.04735.x
Christudoss, P., Selvakumar, R., Fleming, J. J., & Gopalakrishnan, G. (2011). Zinc status of patients with benign prostatic hyperplasia and prostate carcinoma. Indian journal of urology : IJU : journal of the Urological Society of India, 27(1), 14–18. https://doi.org/10.4103/0970-1591.78405
Men, C., Wang, M., Aiyireti, M., & Cui, Y. (2016). The efficacy and safety of Urtica dioica in treating benign prostatic hyperplasia: A systematic review and meta-analysis. African Journal of Traditional, Complementary and Alternative Medicines, 13 (2), 143-150. http://dx.doi.org/10.4314/ajtcam.v13i2.17
Ngai, H. Y., Yuen, K. S., Ng, C. M., Cheng, C. H., & Chu, S. P. (2017). Metabolic syndrome and benign prostatic hyperplasia: An update. Asian journal of urology, 4(3), 164–173. https://doi.org/10.1016/j.ajur.2017.05.001
Robert, G., Descazeaud, A., Nicolaïew, N., Terry, S., Sirab, N., Vacherot, F., Maillé, P., Allory, Y., & de la Taille, A. (2009). Inflammation in benign prostatic hyperplasia: a 282 patients’ immunohistochemical analysis. The Prostate, 69(16), 1774–1780. https://doi.org/10.1002/pros.21027
Roehrborn C. G. (2005). Benign prostatic hyperplasia: an overview. Reviews in urology, 7 Suppl 9(Suppl 9), S3–S14.
Sarris, J & Wardle, J (2014) Clinical Naturopathy (2nd ed), Elsevier: Australia.
Xia, B. W., Zhao, S. C., Chen, Z. P., Chen, C., Liu, T. S., Yang, F., & Yan, Y. (2020). The underlying mechanism of metabolic syndrome on benign prostatic hyperplasia and prostate volume. The Prostate, 80(6), 481–490. https://doi.org/10.1002/pros.23962